
Fire in the OR™ evidence brief
Published February 8, 2022
This paper discusses the major training challenges professionals face in scaling fire in the OR training to cover large provider populations across health systems. Virtual Reality (VR) provides a new training modality to address training on operating room fires. This paper reviews the challenges associated with traditional training methods and presents the evidence associated with how VR can provide an alternative that is more effective, efficient and economical than traditional training techniques.
SURGICAL FIRE TRAINING CHALLENGES
In the United States, there are an estimated 550-650 surgical fires per year1. And while the number of fires annually may be relatively low as a percentage of total surgeries performed, they have serious consequences. The average claim from a surgical fire that results in patient injury tallies $120,1662, with some awards reaching $30 million3. Losses extend beyond the financial, tarnishing the reputation of and trust in provider entities.
Concern over surgical fire events has prompted leading medical entities to issue guideline statements. The American Society of Anesthesiologists (ASA)4, the Association of Perioperative Registered Nurses (AORN)5, and even the US Food & Drug Administration (FDA)[6], for example, cite training as a key step in preventing and managing surgical fires.
“Education and training in fire risk reduction strategies for perioperative RNs, surgical technologists, anesthesia care providers, surgeons, and other personnel is essential to promote and maintain a firesafe perioperative environment.[7]
There are two main challenges that healthcare educators must overcome.
Challenge #1: Ensuring surgical fire proficiency. Educators may choose from a range of surgical fire training techniques, each with their own strengths and weaknesses. These include grand rounds, simulation training, eLearning or simple reading assignments. Such training may be conducted by facility resources or outsourced to industry educators. Facility training can be problematic because content frequently varies between creators and provider locations. This makes it difficult to achieve a standardized surgical fire proficiency level across a system-wide trainee population.
Legacy surgical fire training options have other drawbacks. These include:
- Manikin-based simulation training. While some simulations leverage real fire, most traditional simulation training techniques don’t because it simply isn’t practical on a large-scale basis. Simulation typically involves the use of manikins and smoke/fog machines. These simulations usually require an hour or more to complete and a significant amount of time to setup. They may be conducted by the in-house staff or outsourced to third-party experts. If the simulation is conducted in an OR, that incurs the additional cost of sidelining an active OR. For these reasons, sustaining a manikin-based simulation program for surgical fire training poses significant operational challenges.
- No training. These difficulties, along with resource-strapped educational programs, lead to the reality that many clinicians never receive effective training on how to prevent and respond to a surgical fire.
- eLearning training. eLearning content can be an important tool to communicate protocols and safety information. However, eLearning programs do not impart the hands-on experiences necessary for learners to prepare for this high-stakes patient safety situation. Unfortunately, eLearning programs tend to be the only cost-effective learning modality for fire training at a large scale.
“Since the occurrence of an OR fire event is relatively uncommon, simulation plays a key role in training the OR team for preparedness.”[8]
Challenge #2: Delivering cost-effective training. Legacy surgical fire training approaches are an expensive task. Simulation management activities are resource intensive, consuming inordinate labor hours to manually assign, schedule, run, teach, track and report proficiency results for trainees. Furthermore:
- Legacy solutions are difficult to scale across large learner populations. This is problematic for health care systems with hundreds of surgeons, nurses, technicians and anesthesiologists who require surgical fire training.
- Legacy solutions are not mobile — they can’t easily be moved and set up at various locations. This is not ideal for health systems with multiple, and geographically-disparate, locations. Consequently, trainees must travel to a simulation center for training, which results in additional commuting and backfilling expenditures as well as schedule coordination difficulties.
“Immersive learning environments that use virtual simulation (VS) technology are increasingly relevant as medical learners train in an environment of restricted clinical training hours and a heightened focus on patient safety.”[9]
EVIDENCE SUPPORTING SURGICAL FIRE VR TRAINING
The global VR market in healthcare is projected to rise at a compound annual growth rate of 54.5 percent from 2017-202310Moreover, the global VR market in healthcare is projected to reach US$ 5.1 billion by 202511. These figures are underscored by significant adoption of VR technologies for healthcare education and simulation as a new modality.
“Interactive VR-based hands-on training was found to be a relatively inexpensive and effective mode for teaching12.”
VR-based OR fire training simulation study13
This 2018 study published in Surgical Endoscopy compared a headset-mounted, immersive VR-based OR fire training simulation system to traditional reading/lecture training.14
Study findings:
- The VR simulation group performed 250% better at putting out a mock OR fire using the correct order of steps (7/10 participants) versus the control group (2/10 participants.) This suggests that the study group is better suited to transfer the VR training to clinical practice in a real fire.
- “The VR simulation group could correctly identify oxidizer sources more than the control group.” Thus, they demonstrated a superior grasp of the fire triad, which is critical to preventing fires.
These findings demonstrate the effectiveness of VR surgical fire simulation and the feasibility of employing this training modality. VR kiosks can be integrated into the onboarding process for new peri-operative hires and for sustaining competency.
A similar study identified a trainee preference for the VR training mode, where 67% of participants, “…chose the virtual OR fire trainer over the traditional training methods15.” This led researchers to conclude that:
“Training for OR fire emergencies in fully immersive virtual reality environments may be the ideal training modality.”16 [Emphasis added]
Health Scholars’ Fire in the OR VR simulation user survey
This data comes from user participants who responded to the Health Scholars’ Fire in the OR VR simulation user survey (n=34). The survey was completed during beta testing of Health Scholars’ Fire in the OR VR Simulation at three major health care organizations in the United States in 2018.
“The Health Scholars’ Fire in the OR VR simulation solution was immersive, detailed, and pretty realistic. Much more applicable to real life scenarios than a PEAK module or other passive online learning.”17
Respondent roles ranged across surgeons, nurses/techs, anesthesiologists, residents and fellows in hospital settings. Users completed the Fire in the OR’s three modules as described below.
1-Tutorial Module (8 minutes)
- Teaches how to use the VR system and perform key actions so that non-gamer professionals can complete the simulation with confidence.
2-Fire Triad Module (6 minutes)
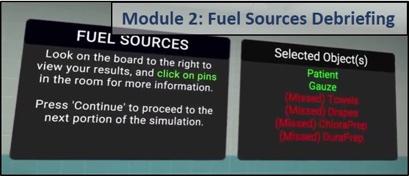
- Teaches how to identify items in the OR that contribute to surgical fires as part of the Fire Triad (fuel sources, oxidizers, and ignitors). Gives feedback on selections. A pass/no pass score is assessed and users are able to repeat as needed.
- Integrates a self-guided debriefing, i.e. an instructor need not be present. One study found this approach, may be “equivalent” to facilitator-led debriefing.18
3-Fire on a Patient Module (8 minutes)
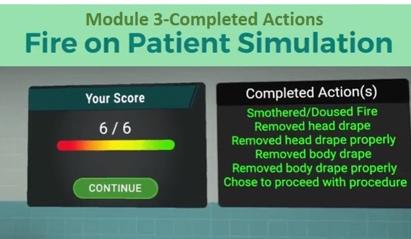
- The simulation is based on a real-world case and calls upon trainees to extinguish a fire on a patient and follow through with other tasks to ensure patient safety. Users are scored (pass/no pass) on their actions and they are debriefed dynamically with a self-guided debriefing mechanism.
Total training time: 20 – 25 minutes, and may be immediately reset for the next iteration.
Survey findings:
- 71% found the immersive VR experience so realistic that they “lost” themselves in the simulation.
“…the retention level a year after a VR training session can be as much as 80%, compared to 20% retention after a week with traditional training.”19 Dr. Narendra Kini, CEO at Miami Children’s Health System
- 100% of participants said that the Health Scholars’ fire in the OR VR simulation would “enhance,” or could be used to “replace,” current training modes.
WHY VR SOLVES THE LIMITATIONS OF CURRENT TRAINING
The evidence above supports the adoption and use of VR solutions to supplement and expand surgical fire training across health systems. VR fire in the OR applications overcome many of the legacy training challenges detailed above, including:
- It’s a more effective teaching tool. VR promotes better learning outcomes and in the Surgical Endoscopy study proved to be dramatically more effective in training all the fire steps in the right order. VR applications incorporate psychomotor actions, such as removing an inflamed surgical drape, to build muscle memory. This is superior to eLearning and reading alternatives.
- VR is portable and takes less time to set up. The portability of VR applications make them easy to take to learner locations, which reduces trainee travel time and expense. Hardware is simple to set up and with just a few steps applications are up and running, easing the administrative burden of setting up a simulation.
- Simulations are easily repeatable. The low-cost, easy to setup and administer clinical fire VR applications support sustainability training goals. Short maintenance training can readily be repeated every 6-12 months.
“…the advantages of VEs [virtual environments] over other immersive learning techniques (including convenience, scalability, cost, and distributability) are undeniable.”20
- Overall, VR can cost up to 50% less than traditional simulation for clinical fire training. Fire in the OR VR simulation applications make use of low-cost-equipment, hardware and software. They don’t require expensive manikins, nor do they sideline precious OR facilities.
- For example, traditional clinical fire training techniques could easily cost $300 per person per year — or $150,000 for a trainee population of 500, excluding facility costs. The use of a fire in the OR VR application could conservatively cut this cost by 50% — down to $50,000 per year, or $150 per person. This includes all expenses for software, hardware and trainee labor hours.
SUMMARY
Virtual simulation (VS) environments add convenience and flexibility and increase the ability to scale and distribute simulations widely with lower costs.”21
Fire in the OR educators considering VR applications may be comforted by the facts that:
- VR is a more effective way to train. The evidence cases above show that immersive fire in the OR simulations are more effective in promoting surgical fire proficiency — by 250% according to the Surgical Endoscopy study.
- VR is a more operationally- and cost-efficient way to train. Fire in the OR VR applications are scalable across health systems by taking advantage of highly portable VR hardware solutions. Thus, simulation and education managers can quickly set it up in a small space near trainee populations to minimize time lost due to travel. Additionally, surgical fire VR training applications are cost effective. As a result, budget-strapped educators are able to deliver surgical fire training at up to 1/2 the cost of traditional training techniques.
- It’s an enjoyable way to learn. Our survey, along with other evidence cited above, shows that users find VR engaging, valuable, and prefer the use of this VR-based training mode.
About Health Scholars
Health Scholars was founded by healthcare professionals who recognized the need to advance immersive education and clinical training effectiveness. Our mission is to improve patient safety via the delivery of experiential learning and advanced simulation to nurses, physicians and team-based healthcare staff via a single, future ready education platform. One that is easy to use, is scalable across a health system, and more effectively manages, delivers and analyzes blended learning programs.
The Health Scholars One Blended Learning Platform delivers advanced learning technologies, methodologies and the best mix of modern and engaging content, including virtual reality simulations. It improves the efficiency of delivering blended learning programs, and combined with interactive content solutions, improves the effectiveness of education programs.
Health Scholars is headquartered in Denver, Colorado and has clinical and support operations embedded in the world-class Jump Trading Simulation and Education Center on the OSF Campus in Peoria, Illinois.
To Learn More
Contact us today to learn how our Fire in the OR™ VR simulation can help you:
- Promote OR fire competency.
- Significantly reduce fire in the OR training costs and have a tool to demonstrate proficiency.
- Deliver consistent, standardized training across health systems and educational campuses.
https://healthscholars.com/ | email: info@healthscholars.com | Ph: 888.584.8845
1 “ECRI Institute New Clinical Guide to Surgical Fire Prevention.” Health Devices, October 2009. 2 Mehta, SP; Bhananker, SM; Posner, KL; et al, “Operating Room Fires: A Closed Claims Analysis”, Anesthesiology, May 2013. 3 Rosenfeld J, “Hospital and Doctors Found Liable for Surgical Fire that Left Women Speechless”, Personal Injury New & Developments, April 2015. 4 “Practice Advisory for the Prevention and Management of Operating Room Fires,” Anesthesiology, V 118 • No 2, February 2013. See “Advisories” on p. 274. 5 “AORN Guidance Statement: Fire Prevention in the Operating Room,” AORN, 2005. 6 “Recommendations to Reduce Surgical Fires and Related Patient Injury: FDA Safety Communication,” U.S. Food & Drug Administration, May 29, 2018. 7 “AORN Guidance Statement: Fire Prevention in the Operating Room,” AORN, 2005, p. 1. 8 Sankaranarayanan, Ganesh; Wooley, Lizzy; Hogg, Deborah; et al., “Immersive virtual reality-based training improves response in a simulated operating room fire scenario,” Surgical Endoscopy, January 25, 2018, p.2. 9 McGrath, Jillian, L, MD; Taekman, Jeffrey, M., MD; Dev, Parvati, PhD, “Using Virtual Reality Simulation Environments to Assess Competence for Emergency Medicine Learners,” The Society for Academic Emergency Medicine, 2017, p. 1. 10 “Virtual Reality (VR) in Healthcare Market: Global Industry Analysis, Trends, Market Size and Forecasts up to 2023,” Research and Markets, March 2018. 11 “Healthcare Augmented & Virtual Reality Market Worth $5.1 Billion By 2025,” Grand View Research, Inc., May, 2017. 12 Sankaranarayanan, Ganesh; Wooley, Lizzy; Hogg, Deborah; et al., “Immersive virtual reality-based training improves response in a simulated operating room fire scenario,” Surgical Endoscopy, January 25, 2018, p. 1. 13 Sankaranarayanan, Ganesh; Wooley, Lizzy; Hogg, Deborah; et al., “Immersive virtual reality-based training improves response in a simulated operating room fire scenario,” Surgical Endoscopy, January 25, 2018, p. 1. 14 Note that this study is not based on Health Scholars’ VR simulation. That said, Health Scholars engaged the same designer to build its VR simulation and we therefore believe that they are at least comparable. 15 Dorozhkin, D; Olasky, J; Jones, DB, et al. “OR fire virtual training simulator: design and face validity.” Surgical Endoscopy, Sept. 2017, 31(9): p. 3262. 16 Dorozhkin, D; Olasky, J; Jones, DB, et al. “OR fire virtual training simulator: design and face validity.” Surgical Endoscopy, Sept. 2017, 31(9): p. 3263. 17 Resident participant, “Health Scholars’ Fire in the OR Beta Survey,” Health Scholars, June, 2018. 18 Oikawa, Savaka, M.D.; Berg, Benjamin, M.D.; Turban, Joseph, M.D.; et al. “Self-Debriefing vs Instructor Debriefing in a Pre-Internship Simulation Curriculum: Night on Call.” Hawaii J Med Public Health, 2016 May; 75(5): 127-132, see Conclusions. 19 Note that she is not referring specifically to the Health Scholars’ Fire in the OR VR solution. Gaudiosi, John, “Here's why hospitals are using virtual reality to train staff,” FORTUNE, August 17, 2015. 20 Taekman, J.M.; Shelley, K. “Virtual environments in healthcare: immersion, disruption, and flow.” Int Anesthesiol Clin, 2010; 48: p. 104. 21 McGrath, Jillian, L, MD; Taekman, Jeffrey, M., MD; Dev, Parvati, PhD, “Using Virtual Reality Simulation Environments to Assess Competence for Emergency Medicine Learners,” The Society for Academic Emergency Medicine, 2017, p. 1.





